Nitric Oxide and Hormones
1 year, 6 months ago
9188
0
Posted on Jan 26, 2023, 4 p.m.
Nitric oxide (NO) supports homeostasis in the endothelium. Endothelial cells are cells that line the interior surface of blood vessels or lymphatic vessels. Vascular endothelial cells line the entire circulatory system, from the heart to the smallest capillaries. Decreased production of NO disrupts this homeostasis and increases the risk for several conditions like cardiovascular disease, hypertension, blood clotting, and inflammation.
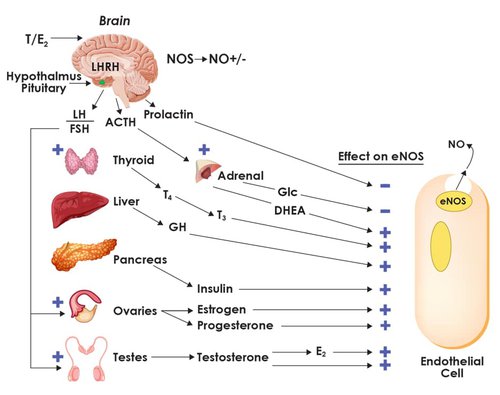
Hormones have a strong effect on the pathways that stimulate NO production. Likewise, the presence of NO plays a role in some hormone regulation.
Aging is the loss of hormones. Aging is the loss of nitric oxide.
The Effects of Aging on Hormones and Nitric Oxide Production Several hormones positively stimulate endothelial Nitric Oxide Synthase (eNOS) in the production of NO. These hormones include:
- Estrogen
- Testosterone
- Progesterone
- DHEA
- Insulin
- Growth Hormone
- Triiodothyronine (T3)
Hormone production naturally declines as part of the aging process. As a result, this combined with other factors of aging causes eNOS function to decrease to around 50 percent by the time a person is 40 years old. By the time a person ages to 60 years old, eNOS only functions at 15% of capacity.
Figure 1 on the following page illustrates how hormones play a role in endothelial health and the potential impact on eNOS functionality. This document can be used for reference or to stimulate further conversation about necessary action to maintain NO levels and support cardiovascular health. Nitric Oxide regulates hormone release in the hypothalamic-pituitary axis.
Integrated Hormonal Regulation of eNOS
Sex Hormones
Nitric oxide regulates hormone release in the hypothalamic-pituitary axis.
NO triggers the pulsatile release of luteinizing hormone-releasing hormone (LHRH), which mediates luteinizing hormone (LH) release. When LH is released, it stimulates the production of steroid hormones from the testis (testosterone) and the ovaries (estradiol).
Estrogen stimulates eNOS to produce nitric oxide.
However, estrogen declines with age. This results in a noticeable decrease in eNOS function around the time of menopause. As a result, 85 percent of women in the US are hypertensive by the age of 85.
When available, estrogen also suppresses oxidative stress. As less NO is needed to scavenge superoxide, this occurrence increases NO’s bioavailability.
Progesterone.
Progesterone acts directly on epithelial cells of the endometrium to stimulate the expression of eNOS.
It also stimulates the phosphorylation of eNOS increasing the production of NO.
Testosterone deficiency induces endothelial dysfunction.
Deficiency can lead to erectile dysfunction and/or vascular dysfunction. Testosterone has a dual action in the modulation of the NO cyclic signaling GMP pathway. Testosterone has been shown to regulate the NO/cGMP pathway, which directly influences endothelial function and endothelial progenitor cells (EPCs). These cells are key for the endothelial repair system. Testosterone also modulates the phosphodiesterase 5 (PDE5) activity in penile tissue.
Aromatase inhibitors impair endothelial function.
Estrogen derived from aromatase has vital effects on NO production and endothelial function. However, aromatase inhibitors such as letrozole and anastrozole hinder estrogen production. Not only are aromatase inhibitors used in breast cancer treatment, but they are also frequently added to compounded prescriptions of testosterone replacement therapy for men.
Adrenal Glands
The adrenal glands require adequate nitric oxide to work effectively.
Glucocorticoid production in the adrenal glands is increased in the absence of NO.
Cortisol is the only hormone that naturally increases with age. All of this has the effect of:
- Inhibiting iNOS, thus impairing immune response
- Inhibiting eNOS, thus causing cardiovascular complications such as hypertension and blood clotting
- Increased reactive oxygen species (ROS) produced by mitochondria, NADPH oxidase (NOX), and xanthine oxidase. This increases oxidative stress thereby decreasing the production of NO
- Decreased synthesis of BH4 which increases NOS uncoupling, resulting in increased oxidative stress and decreasing the production of NO
- Decreased membrane transport of L-arginine thus decreasing the substrate for NOS
DHEA is a prohormone that can be metabolized into other estrogens and testosterone.
It is synthesized in the adrenal cortex, gonads, adipose tissue, brain, and skin. It directly increases NO production by the activation of eNOS.
Low DHEA levels are associated with a higher risk of ED in men and low sexual responsiveness in women.
Pituitary Gland
Growth Hormone (GH) and IGF1 stimulate eNOS.
Adult hypo-pituitarism and untreated GH deficiency are associated with endothelial dysfunction, decreased NO production, increased peripheral resistance, and increased cardiovascular mortality and morbidity.
Oxytocin affects sexual health.
Oxytocin induces penile erection by increasing NOS activity in the cell bodies of oxytocinergic neurons, projecting to extra-hypothalamic brain areas and mediating the behavioral responses.
Oxytocin, the ‘love hormone,’ increases NO production through the NOS enzyme system and levels are greatly increased after an orgasm in both men and women.
Nitric Oxide could extend fertility.
NO appears to slow or reverse the aging of eggs in mouse ovaries. This finding suggests
NO may help women in their 30s and 40s remain fertile longer and increase their chances of having healthy babies.
Metabolic System
NO regulates carbohydrate metabolism and insulin production.
NO is also emerging as a central regulator of energy metabolism and body composition. Impairment of NO synthesis is a central defect causing metabolic abnormalities associated with insulin resistance. Appropriate amounts of insulin will stimulate NOS activity but inappropriate amounts of insulin, as in insulin resistance, decrease NOS activity. Increasing NO output has remarkable effects on obesity and insulin resistance. For example, NO helps activate GLUT4 receptors for the transport of glucose into the cells.
Insulin stimulates eNOS activity, which is vital for NO production in the endothelium.
Insulin resistance decreases eNOS phosphorylation which increases NOS uncoupling.
This contributes to the loss of endothelial function and increases the expression of vascular cell adhesion molecule 1 (VCAM 1) and other adhesion molecules increasing cardiovascular complications.
Polycystic Ovarian Syndrome
Polycystic Ovarian Syndrome (PCOS) is correlated to insulin resistance, diabetes, obesity, oxidative stress, inflammation, and cardiovascular disease. All of these conditions are mediated by NO. PCOS can have the following effects on the body:
- Increased oxidative stress and NOS uncoupling decreasing NO levels
- Decreased T regulatory cells which modulate the immune system, maintain tolerance to self-antigens, and prevent autoimmune disease. These are known to be regulated by NO levels.
- Increased asymmetric dimethylarginine (ADMA) synthesis which decreases arginine bioavailability. Arginine is converted by healthy eNOS into NO.
- Increased ADMA uncouples NOS, decreasing NO Production and increasing superoxide production.
- ADMA competes with L-arginine for its place in the NOS enzyme thus decreasing the production of NO.
Thyroid
Cold extremities as a symptom in individuals with thyroid imbalance may be a result of NO deficiency.
In the thyroid, NADPH oxidase (NOX) enzymes called DUOX1 and DUOX 2 increase the generation of ROS (reactive oxygen species), such as superoxide and hydrogen peroxide. This is important because a precise amount of hydrogen peroxide is required for thyroid peroxidase (TPO) to function optimally. Increased DUOX activity, along with reduced TPO activity, has deleterious effects on the thyroid tissue caused by oxidative stress. Several factors such as environmental toxicities, mast cell activation, stress, chronic infections, or inflammation contribute to the upregulation of NOX and DUOX, which increases ROS. However, NO and nitrites inhibit NOX and the DUOX enzymes. Supporting the nitrate to nitrite to NO pathway may be an underutilized thyroid therapy due to its role in decreasing the production of superoxide and other ROS by optimizing NO levels, scavenging ROS, and supporting healthy circulation and microcirculation.
Circadian Rhythm
Decreased NO from aging is linked to impaired circadian rhythm
Reduced NO production contributes to age-associated impairment of clock gene expression. Basically, impairment of NO production results in a phase shift of the circadian clock. When circadian rhythmicity is impaired, a condition called non-dipper hypertension can occur. This refers to when blood pressure does not decrease nocturnally as it should. Non-dippers experience impaired endothelial-dependent vasodilation, attributed to a decrease in NO production. This increases the risk of cardiovascular disease.
Final Thoughts
By the time we are 40, our ability to produce NO through the arginine/NOS pathway decreases to 50%. By the time we are 60, it has decreased to 15%. Supporting the nitrate-to-nitrite-to-NO pathway facilitates the optimal production of NO to prevent many age-related diseases. Nitrate supplementation also supports the recoupling of the NOS enzyme, therefore increasing its functionality to produce more NO and decrease oxidative stress.
“Aging is the loss of hormones. Aging is the loss of NO.”
—Beth Shirley RPh, CCN
For more information:
Email: info@berkleylife.com
Call: +1-310-505-3896
This article was provided by Carol Petersen RPH, CNP, and CEO of The Wellness By Design Project, and it was written by Beth Shirley RPH, CCN.
As with anything you read on the internet, this article should not be construed as medical advice; please talk to your doctor or primary care provider before changing your wellness routine. This article is not intended to provide a medical diagnosis, recommendation, treatment, or endorsement.
Opinion Disclaimer: The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy of WHN/A4M. Any content provided by guest authors is of their own opinion and is not intended to malign any religion, ethic group, club, organization, company, individual, or anyone or anything.
Content may be edited for style and length.
References/Sources/Materials provided by:
https://thewellnessbydesignproject.com/nitric-oxide-and-hormones/
- Całka J. The role of nitric oxide in the hypothalamic control of LHRH and oxytocin release, sexual behavior and aging of the LHRH and oxytocin neurons. Folia Histochem Cytobiol. 2006;44(1):3-12.
- Ghasemi A, Zahediasl S. Is nitric oxide a hormone?. Iran Biomed J. 2011;15(3):59-65.
- Sansbury BE, Hill BG. Regulation of obesity and insulin resistance by nitric oxide. Free Radic Biol Med. 2014;73:383-399. doi:10.1016/j.freeradbiomed.2014.05.016
- Sansbury BE, Hill BG. Regulation of obesity and insulin resistance by nitric oxide. Free Radic Biol Med. 2014;73:383-399. doi:10.1016/j.freeradbiomed.2014.05.016
- Nath, P., & Maitra, S. (2018). Physiological relevance of nitric oxide in ovarian functions: an overview. General and Comparative Endocrinology. doi:10.1016/j.ygcen.2018.09.008
- Duckles SP, Miller VM. Hormonal modulation of endothelial NO production. Pflugers Arch. 2010;459(6):841-851. doi:10.1007/s00424-010-0797-1
- Khorram O, Han G. Influence of progesterone on endometrial nitric oxide synthase expression. Fertil Steril. 2009;91(5 Suppl):2157-2162. doi:10.1016/j.fertnstert.2008.05.019
- American Chemical Society. “Nitric Oxide Could Extend Fertility.” ScienceDaily. ScienceDaily, 8 September 2005. <www.sciencedaily.com/releases/2005/09/050908084148.htm>.
- Meng, C. (2019). Nitric oxide (NO) levels in patients with polycystic ovary syndrome (PCOS): a metaanalysis. Journal of International Medical Research, 4083–4094. https://doi.org/10.1177/0300060519864493
- El-Sakka AI. Dehydroepiandrosterone and Erectile Function: A Review. World J Mens Health. 2018 Sep;36(3):183-191. https://doi.org/10.5534/wjmh.180005
- Sansbury BE, Hill BG. Regulation of obesity and insulin resistance by nitric oxide. Free Radic Biol Med. 2014;73:383-399. doi:10.1016/j.freeradbiomed.2014.05.016
- Melis MR, Succu S, Iannucci U, Argiolas A. Oxytocin increases nitric oxide production in the paraventricular nucleus of the hypothalamus of male rats: correlation with penile erection and yawning. Regulatory Peptides. 1997 Mar;69(2):105-111. DOI: 10.1016/s0167-0115(97)00002-5.
- Kunieda, Takeshige & Minamino, Tohru & Miura, Kentaro & Katsuno, Taro & Tateno, Kaoru & Miyauchi, Hideyuki & Kaneko, Shuichi & Bradfield, Christopher & FitzGerald, Garret & Komuro, Issei. (2008). Reduced Nitric Oxide Causes Age-Associated Impairment of Circadian Rhythmicity. Circulation research. 102. 607-14. 10.1161/CIRCRESAHA.107.162230.
- Hotta Y, Kataoka T, Kimura K. Testosterone Deficiency and Endothelial Dysfunction: Nitric Oxide,
Asymmetric Dimethylarginine, and Endothelial Progenitor Cells. Sex Med Rev. 2019;7(4):661-668. doi:10.1016/j.sxmr.2019.02.005
https://www.worldhealth.net/news/nitric-oxide-no-yes-we-want-it/
https://thewellnessbydesignproject.com/review/estrogens-storm-season-stories-of-perimenopause/









